Dr. Sujoy Dasgupta
Obstetrician and Gynecologist, Kolkata
MBBS (Gold Medalist, Hons), MS (Gold Medalist- OBGY), DNB (New Delhi), MRCOG (London), Advanced ART Training for Clinicians (NUHS, Singapore), Fellow- Reproductive Endocrinology & Infertility (ACOG, USA), FIAOG
- 16 Years Experience
- 8 Hospitals
About
- Languages : English, Bengali
Experience
Ex- Clinical Tutor- Obstetrics, Gynaecology, Laparoscopy, KPC Medical College, Kolkata July, 2015 - January, 2016
Consultant, Obstetrics and Gynaecology, Infertility, laparoscopy, Sexual Dysfunction, Upkar Nursing Home, College Street, Kolkata November, 2014 - Present
Ex- Visiting Consultant, Infertility, Sexual Dysfunction, Care IVF Central Avenue, Kokata May, 2013 - Present
Consultant- Obstetrics, Gynaecology, Infertility, laparoscopy, Sexual Dysfunction, Hindusthan Health Point Garia, Kolkata December, 2013 - Present
Consultant- Obstetrics and Gynaecology, Infertility, laparoscopy, RSV Hospital Tollygunj, Kolkata November, 2013 - Present
Visiting Consultant- Obstetrics and Gynaecology, Infertility, laparoscopy, Iris Hospital Baghajatin, Kolkata June, 2014 - Present
Ex- Gynaecologist- Gynaecological Onco-Surgery, Colposcopy, Hysteroscopy, Chittaranjan National Cancer Institute (CNCI), Kolkata July, 2013 - Present
Ex- Incharge, Infertility and IUI, Infertility and IUI Clinic, Medical College Kolkata October, 2010 - Present
Ex- Visiting Consultant, Gynaecology, Infertility, Sexual Dysfunction, Indian Air Force, West Bengal September, 2015 - Present
Ex- Consultant Obstetrics, Gynaecology, Infertility, Laparoscopy, Sexual Dysfunction, Behala Balananda Brahmachary Hospital and Research Centre, Kolkata November, 2015 - Present
Ex- Visiting Obstetrics, Gynaecology, Infertility, Laparoscopy, Zenith Superspecialist Hospital Belgharia, Kolkata June, 2015 - Present
Ex- Visiting Consultant, Infertility, Calcutta Cure Line IVF And Infertility Clinic, Kolkata November, 2015 - Present
Ex- Consultant- Infertility and IVF, Bavishi Pratiksha Fertility Institute Tollygunge, Kolkata September, 2017 - Present
Ex- isiting Consultant- Obstetrics and Gynaecology, Infertility, laparoscopy, AMRI Hospital Mukundapur, Kolkata December, 2017 - Present
Ex- Visiting Consultant- Obstetrics and Gynaecology, Infertility, laparoscopy, Medica Superspeciality Hospital Kolkata, Kolkata December, 2017 - Present
Visiting Consultant- Obstetrics and Gynaecology, Infertility, Laparoscopy, Woodlands Multispeciality Hospital Kolkata, Kolkata January, 2018 - Present
Consultant, Reproductive Medicine, Genome Fertility Centre, Kolkata, Kolkata April, 2018 - Present
Specialities
-
Obstetrics and Gynecology
-
Gynaecological Endoscopy
-
IVF & Infertility
-
Reproductive Medicine
-
Sexology
-
Andrology
-
Gynecology
-
Sexual Medicine
-
Embryology
-
Venereology
-
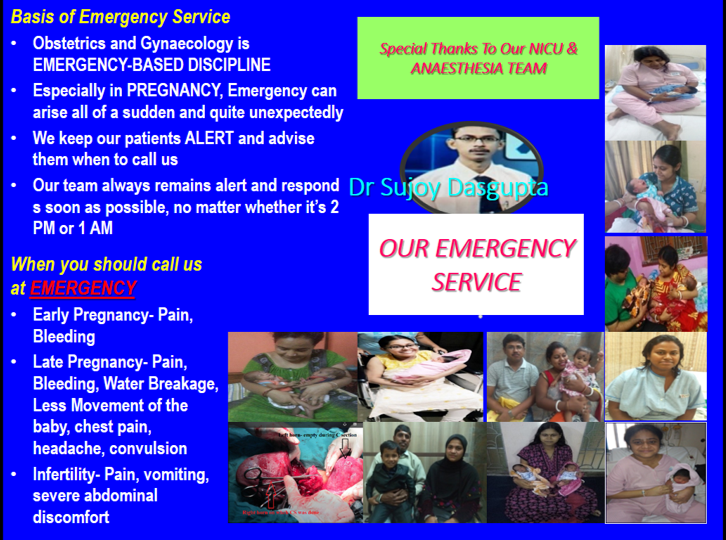
Obstetric Emergency
Procedures
Abdominal Hysterectomy
Ablation
Abortion
Abscess Incision and Drainage
Advanced Laparoscopic Surgery
- More
Conditions
Abnormal Female Sexual Function
Abnormal Menstruation
Abnormal Uterine Bleeding
Abscess
Adrenogenital Disorders
- More
Expertise
2. Consultation
3. Pre-Conceptional Care
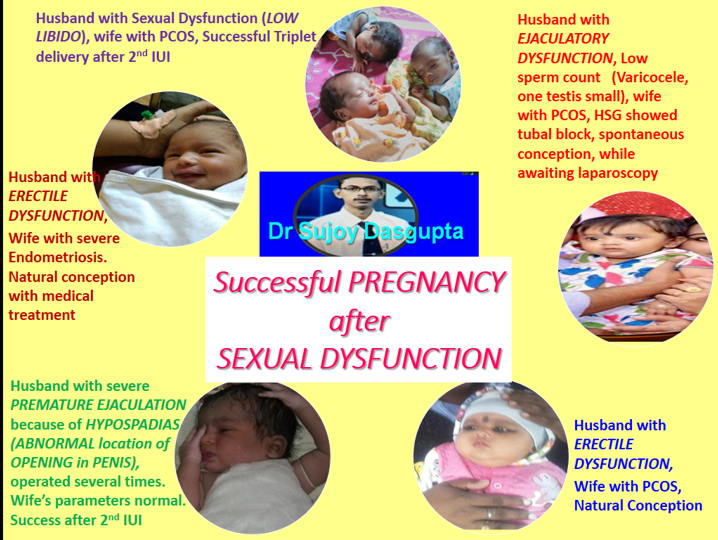
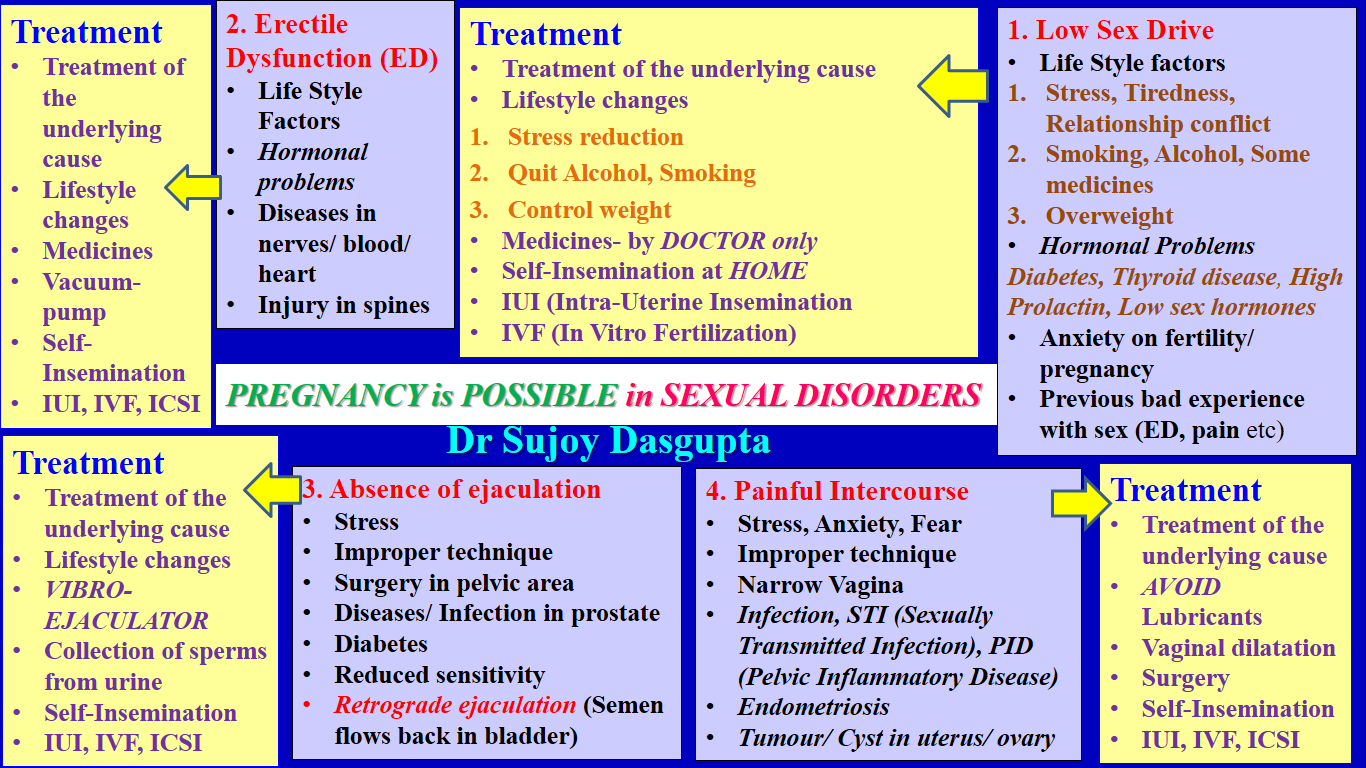
4. Sexual Dysfunction
5. Diagnosis
6. Laparoscopy
7. Hysteroscopy
8. ART (Assisted reproductive technology)- IUI, IVF
9. Treatment for HIV Positive partners
10.Fertility Preservation in Cancer Patient
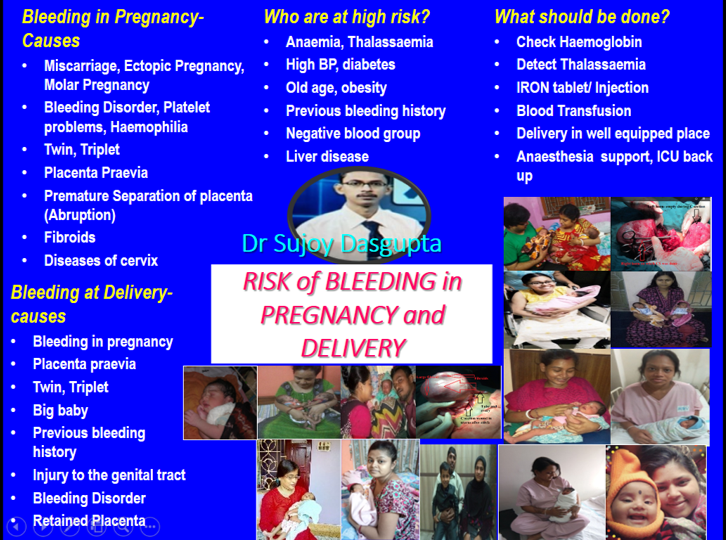
Diagnosis of Infertility
1.Consultation
2.Semen Analysis
3.TVS (Transvaginal Sonography)
4.SSG (Sono-Salpingo-Graphy)
5.HSG (Hystero-Salpingo-Graphy)
6.Hormonal tests
7.Ultrasound Examination
8.Genetic tests- Karyotyping, Y Chromosome Microdeletion
9.Pap Smear
10. Thalassaemia Screening
11.Rubella Screening
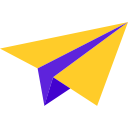
Treatment of Infertility
1.Medicines
2. Ovulation Induction
3. Rubella vaccination
4. IUI (Intrauterine Insemination)
5. IVF (In Vitro fertilization)/ “Test Tube babyâ€
6. Intracytoplasmic Sperm Injection (ICSI)
7. Testicular Biopsy- TESA (Testicular Sperm Aspiration), TESE (Testicular Sperm Extraction), PESA (Percutaneous Epididymal Sperm Aspiration), MESA (Microsurgical Epididymal Sperm Aspiration)
8. Laparo-Hysteroscopy
9. Blastocyst culture
10. PGD (Pre-Implantation genetic Diagnosis)
11. PGS (Pre-Implantation Genetic Screening)
12. Endometrial Scratching
13. Endometrial receptivity Assay (ERA)
14. Sperm Donation
15. Egg Donation
16. Embryo Donation
17. Surrogacy (Altruistic)
18. Sperm freezing
19. Egg Freezing
20. Embryo freezing
Male Infertility
1. Azoospermia
2. Low Sperm Count
3. Sperm Motility problems
4. Sperm Morphology Problems
5. Problems in Semen Viscosity/ Liquefaction
6. Semen Collection problems
7. Ejaculation Problems
8. Absent Ejaculation
9. Retrograde Ejaculation
10. Vibroejaculator
11. Erectile Dysfunction
12. Hormonal treatment
13. Surgical Sperm Recovery
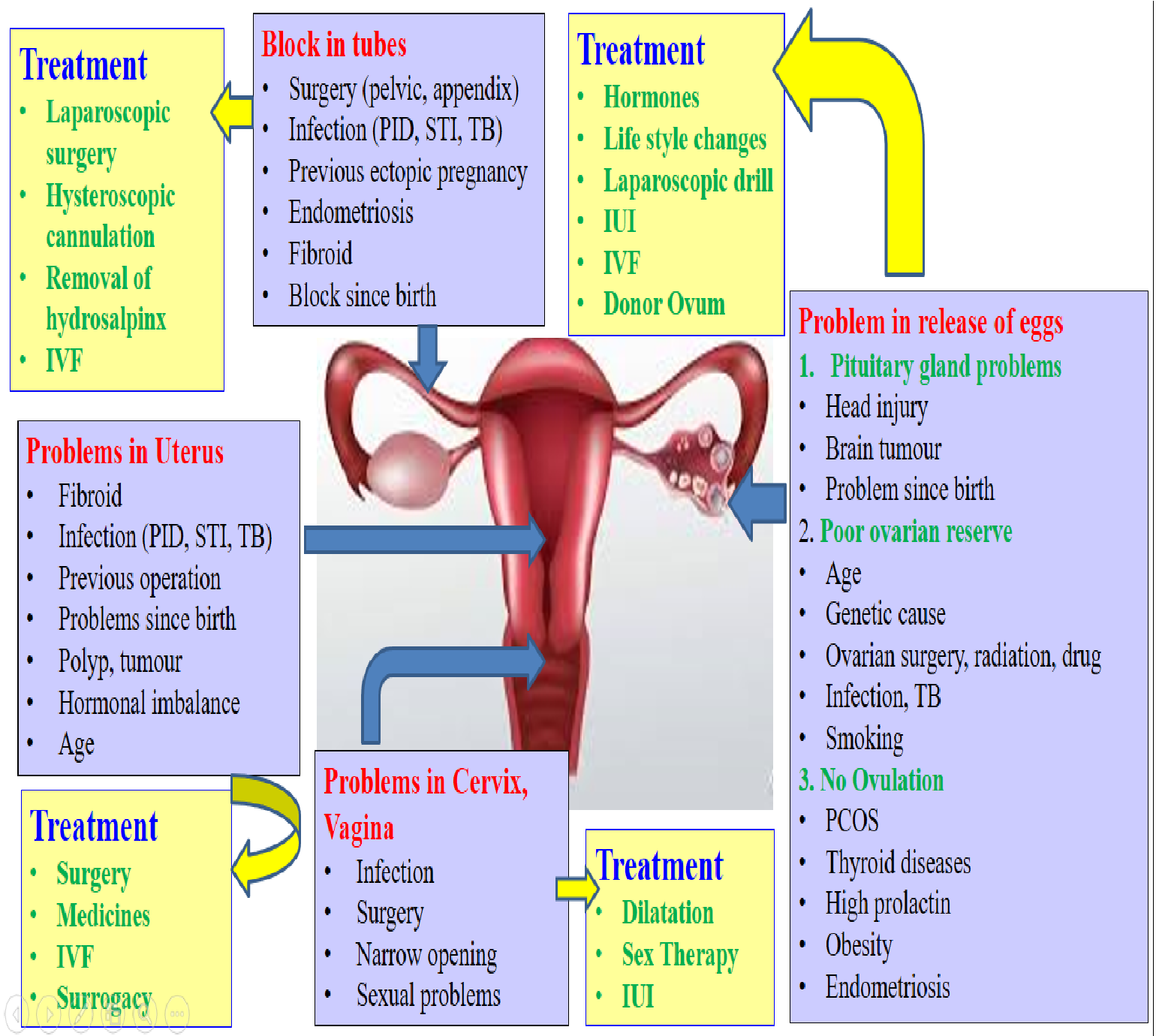
Female Infertility
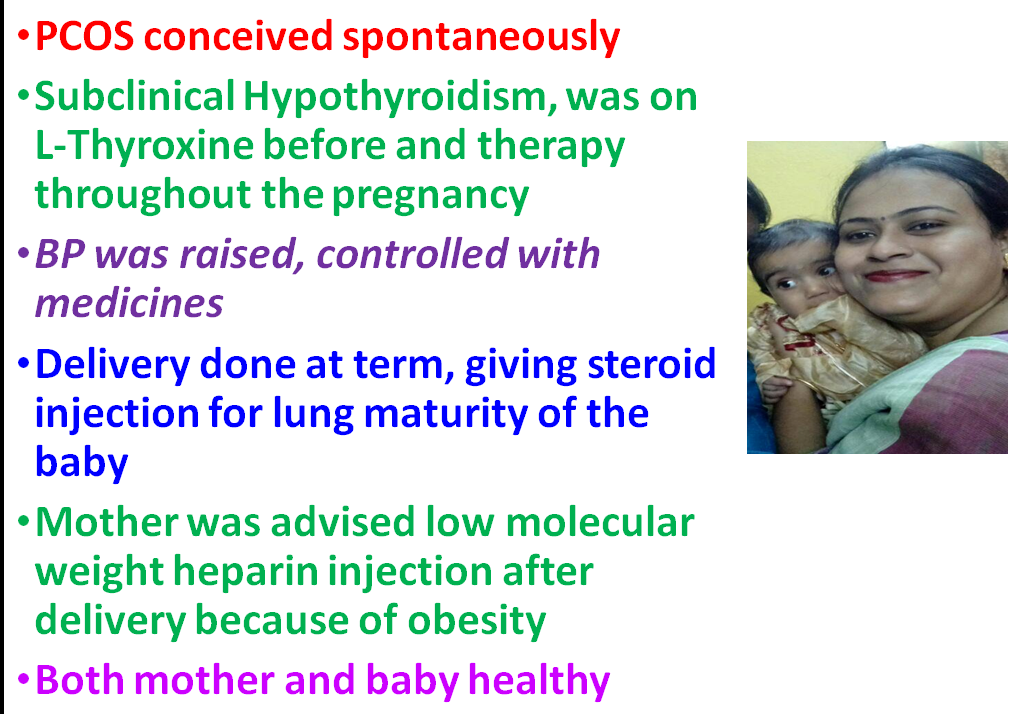
1. PCOS (Polycystic Ovary Syndrome)
2. Endometriosis
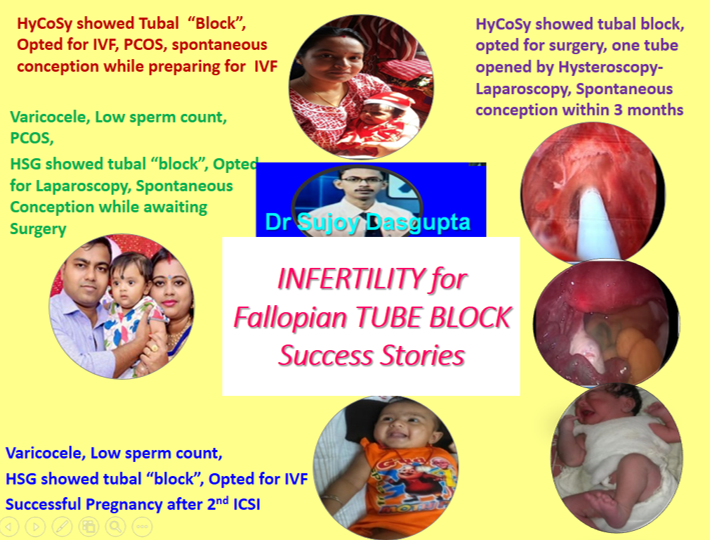
3. Fallopian Tube Block
4. Fibroid
5. Low AMH
6. Poor Ovarian Reserve (POR)
7. Decreased Egg Count
8. Advanced Age
9. Abnormalities in Uterus
10. Sexual Problems
Repeated IVF Failure
1. Medicines
2. Counseling
3. IUI
4. ICSI
5. Blastocyst culture
6. PGD (Pre-Implantation genetic Diagnosis)
7. PGS (Pre-Implantation Genetic Screening)
8. Endometrial Scratching
9. Endometrial receptivity Assay (ERA)
10. G-CSF Injection
11. Sperm Donation
12. Egg Donation
13. Embryo Donation
14. Surrogacy (Altruistic)
Repeated Miscarriage
1. Counseling
2. Consultation
3. Diagnostic Workup
4. Treatment
5. Cervical Cerclage
6. Anti-Phospho-lipid Syndrome
7. PGD (Pre-Implantation genetic Diagnosis)
Pregnancy Care (Obstetrics)
Pre-Pregnancy Planning
1. Counseling
2. Consultation
3. Medicine
4. Diagnostic Workup
Routine Pregnancy care
1. Ante-Natal Care
2. Delivery Service
3. Caesarean Section
4. Emergency Delivery
5. Normal Delivery
6. Post-Natal care
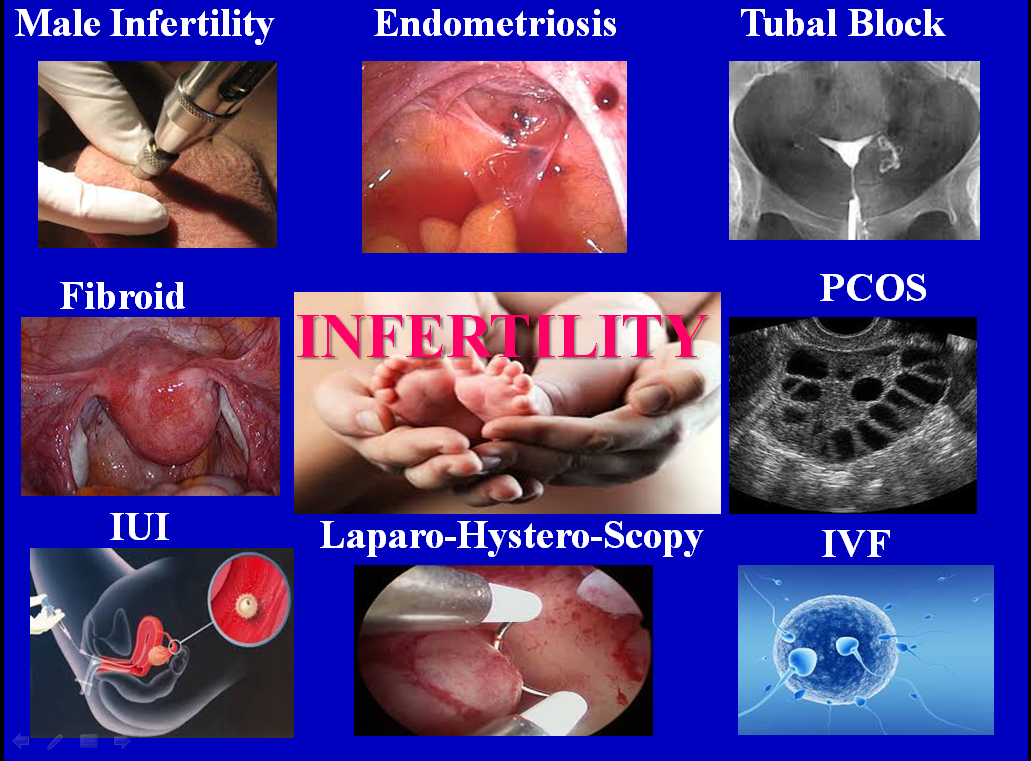
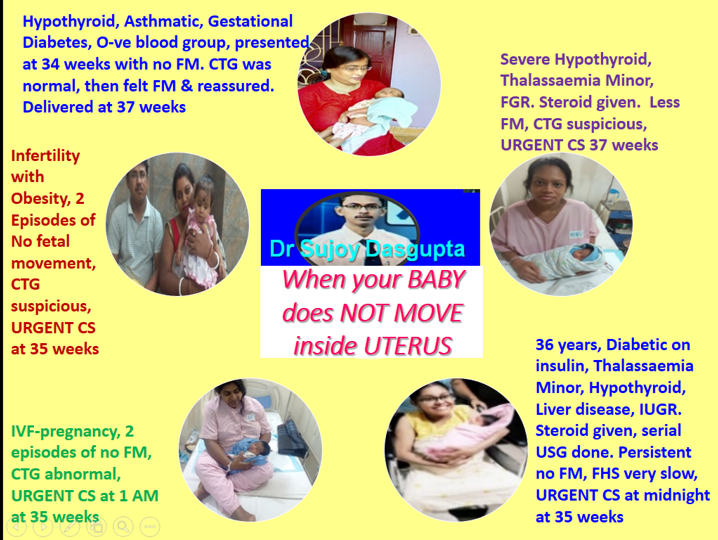
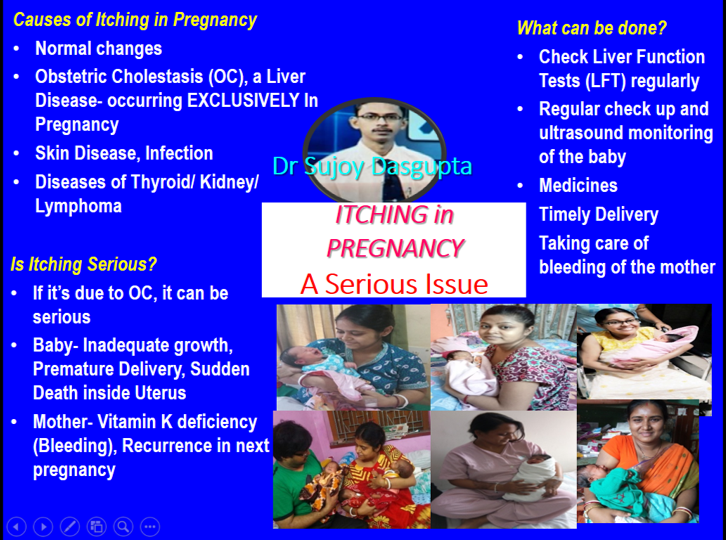
High Risk Pregnancy
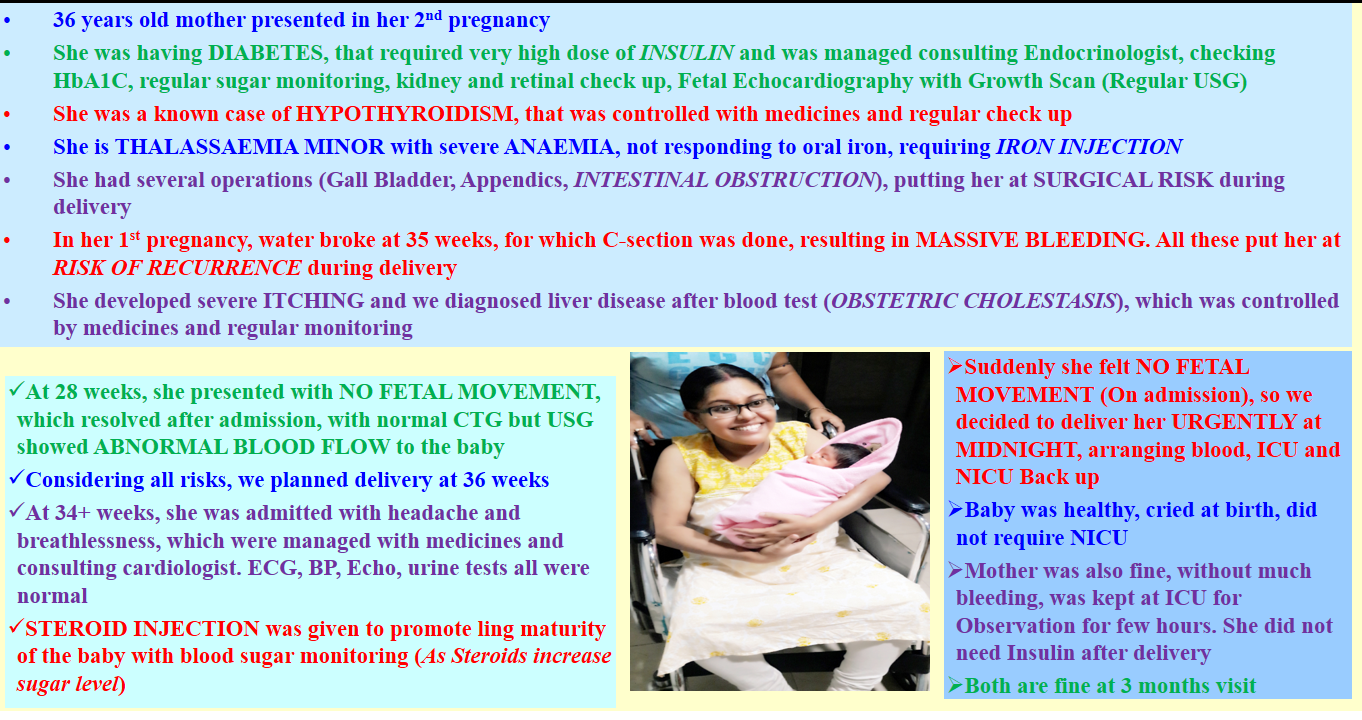
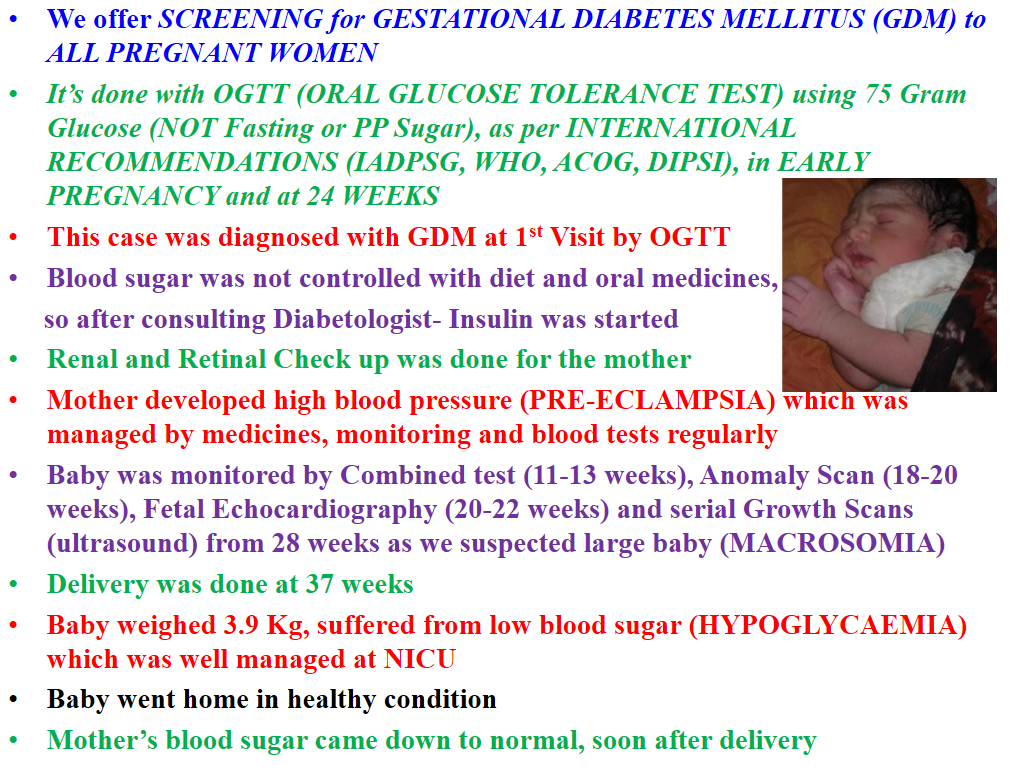
1. Diabetes
2.Hypertension/ Preeclampsia
3.Repeated Miscarriage
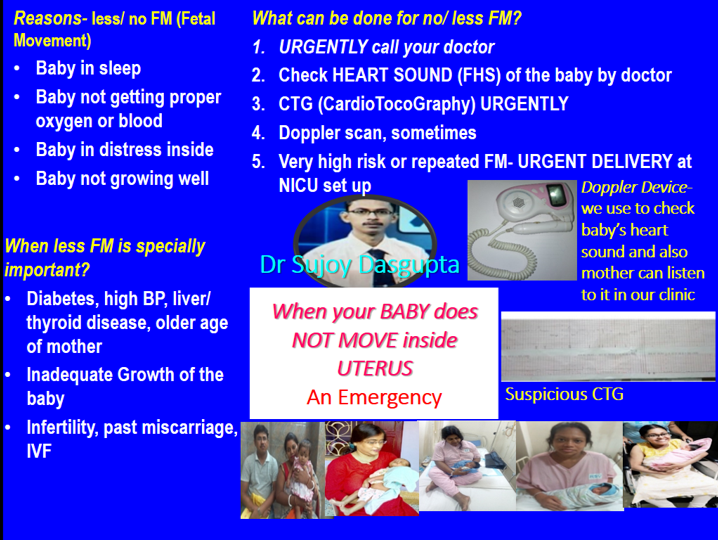
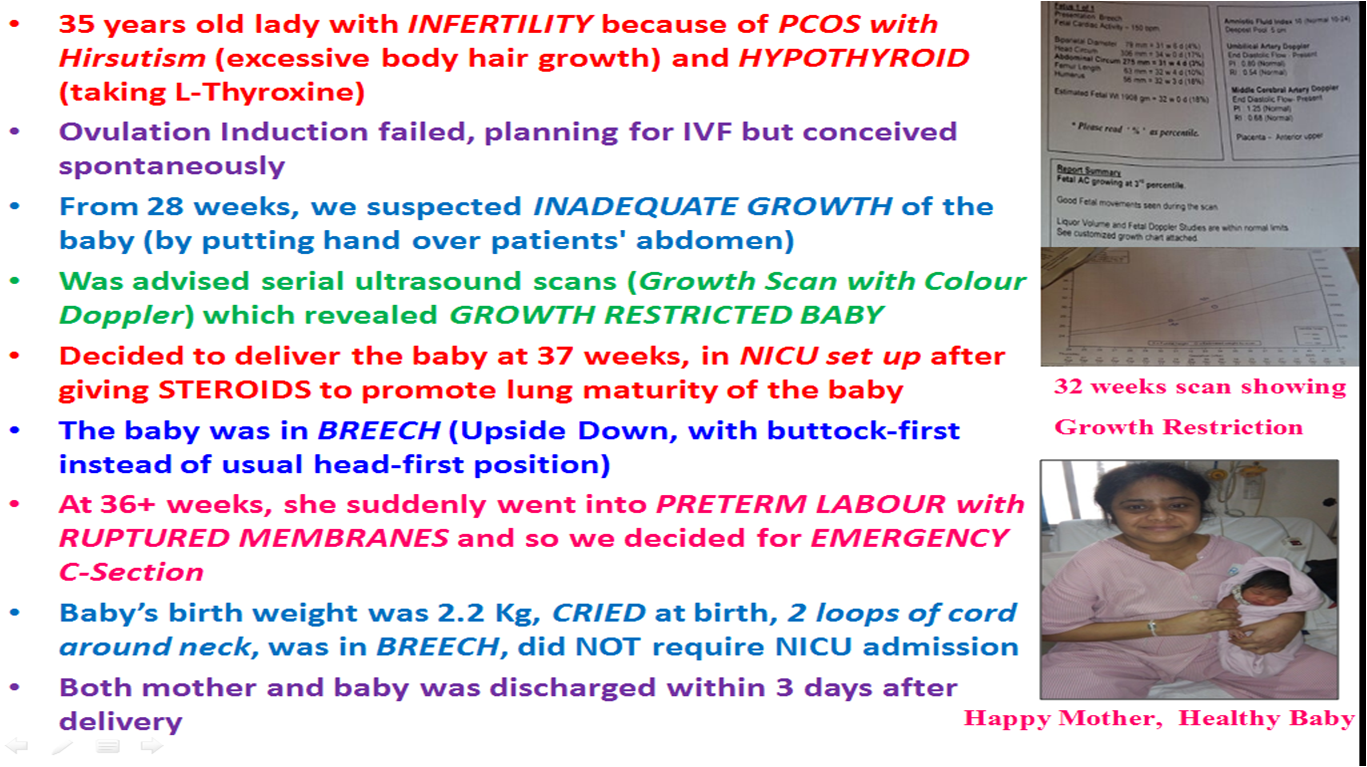
4. Inadequate Growth of the baby (IUGR- Intrauterine Growth restriction)
5. Abnormalities of the baby
6. Fetal Death
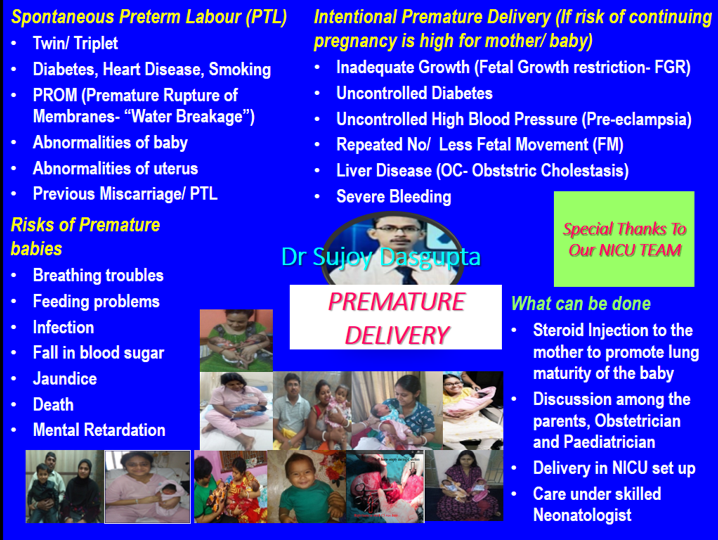
7. Preterm Delivery
8. Cervical Incompetence
9. IVF Pregnancy
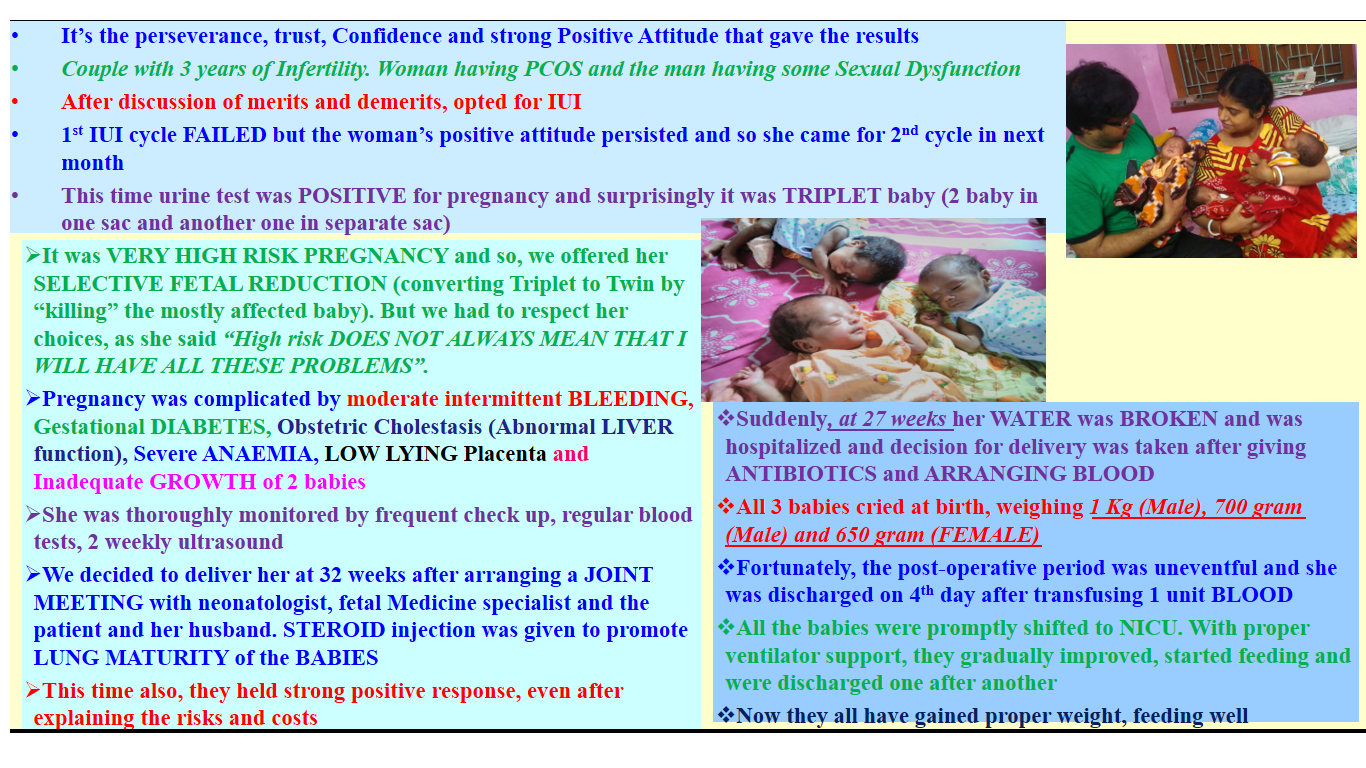
10. Twin/ Triplet Pregnancy
11. Epilepsy
12. Thyroid Diseases
13. Anaemia
14. Thalassaemia
15. Bleeding in Pregnancy
16. Asthma
17. Placenta Praevia
18. Heart/ Liver/ Kidney Diseases
19. ICU Care
20. NICU Service
21. SCBU Service
Emergency Obstetric care
1. Delivery- C Section/ Normal Delivery
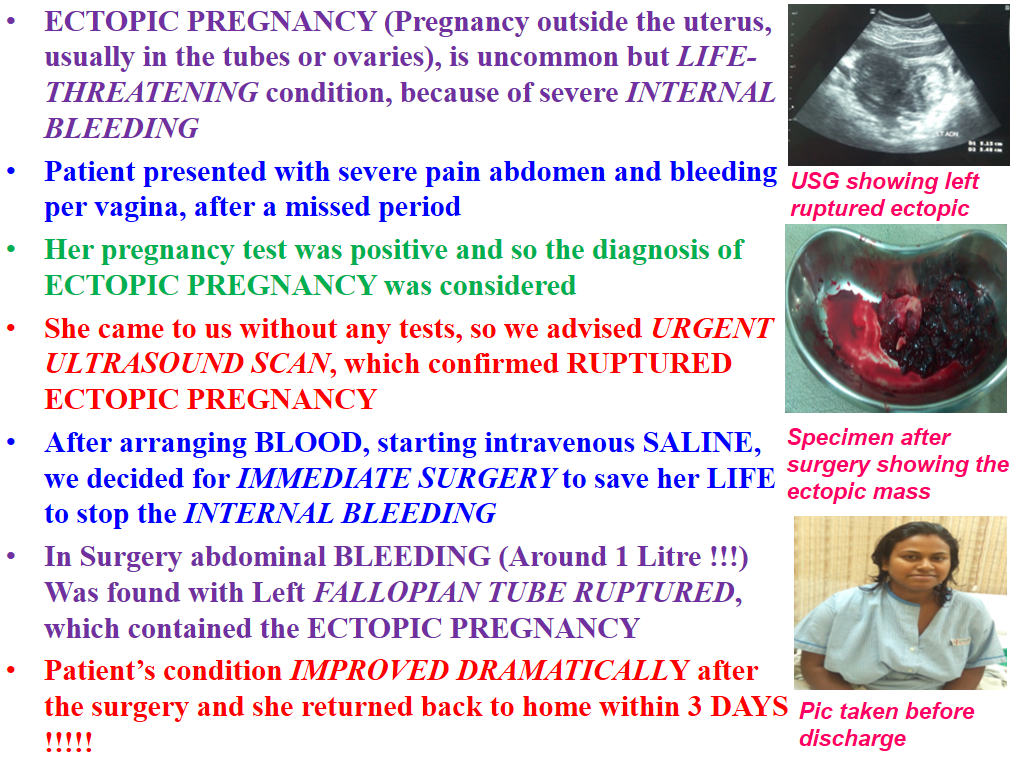
2. Ectopic Pregnancy
3. Miscarriage
4. Cervical Cerclage
5. Dilatation and Evacuation (D/E)
6. Bleeding
7. Eclampsia
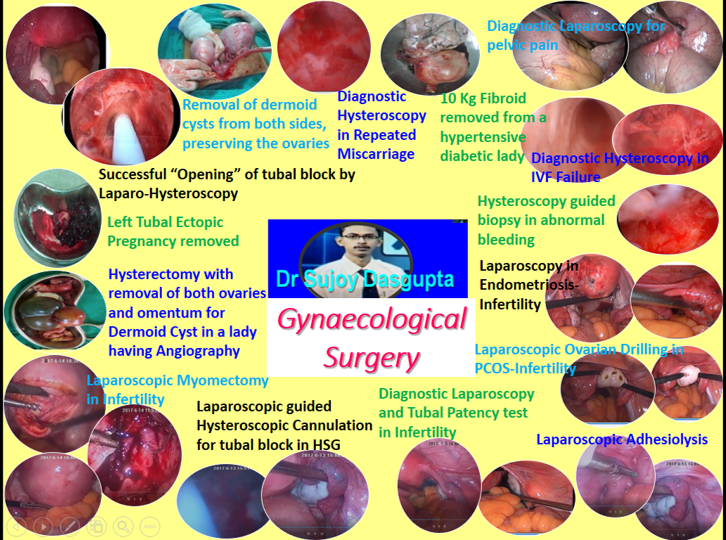
Gynaecological Surgery Laparoscopy
1. Diagnostic laparoscopy
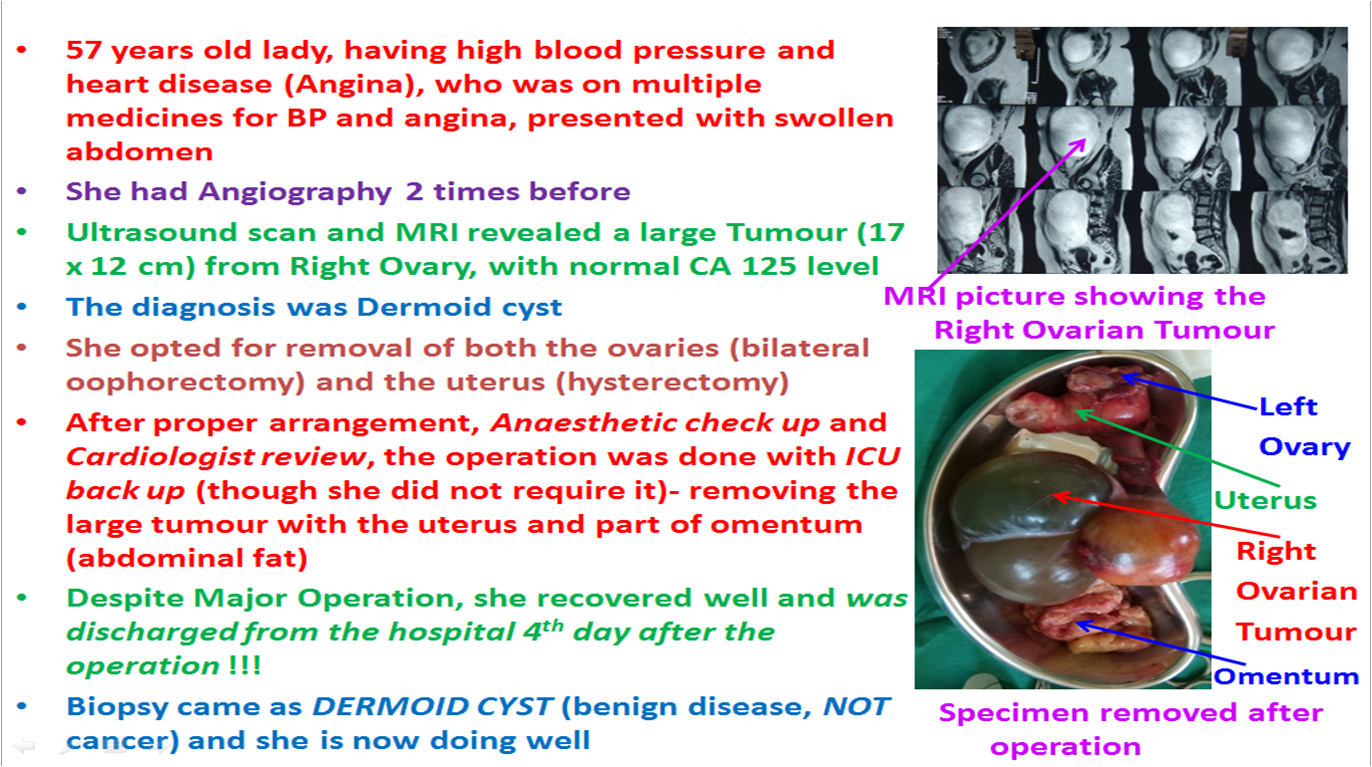
2. Ovarian Cyst
3. Ectopic Pregnancy
4. Tubal Cannulation
5. Adhesiolysis
6. Drilling of polycystic ovaries
7. Surgery for endometriosis
8. Myomectomy (removal of fibroids)
9. Salpingectomy (removal of tubes)
Education
MBBS (Gold Medalist, Hons), 2004, Medical College, Kolkata
MS (Obstetrics and Gynaecology- Gold Medalist), 2010, Medical College, Kolkata
DNB (Obstetrics and Gynaecology), 2014, National Board of Examinations, New Delhi
Fellow- Reproductive Endocrinology and Infertility, 2015, American College of Obstetricians and Gynecologists (ACOG, USA), USA
FIAOG, 2016, Indian Academy of Obstetrics and Gynaecology
MRCOG (London), 2017, Royal College of Obstetricians and Gynaecologists (UK), London
Advanced ART Course for Clinicians (Singapore), 2019, National University Hospital, Singapore
Practice Information

Friends Diagnostic, Kolkata
128, Friends Diagnostic Building, Garia Main Road, Patuli Main Road, Baroda Avenue, Garia, Kolkata, West Bengal - 700084
MON, WED, THU
03:00 PM - 06:00 PM

Saha Polyclinic, Kolkata
Barasat Road, Kachkol More, End of Sodepur Flyover East, Near Sodepur Rail Station Platform Number 4, Sodepur, Kolkata, West Bengal - 700110
SAT
09:00 AM - 01:00 PM

HHP Hospital Pvt. Ltd, Kolkata
Hindusthan More, Near WBSEB, 2406, Garia Main Road, Kolkata, West Bengal - 700084
SAT
03:00 PM - 06:00 PM

RSV Hospital, Kolkata
40, Deshpran Sasmal Road, Tollygunge Phari, Kolkata, West Bengal - 700033
FRI
03:00 PM - 06:00 PM

Genome The Fertility Centre, Shakespeare Sarani
Formerly Theatre Road, Beside Andhra Bank, Near Park Circus Crossing, 67, Shakespeare Sarani, Kolkata, West Bengal - 700017
MON, TUE, WED, THU, FRI
10:00 AM - 02:00 PM

Bhagirathi Neotia Woman & Child Care Centre, Kolkata
2, Rawdon Street, Kolkata, West Bengal - 700017
TUE
05:00 PM - 06:00 PM
.png)
Bhagirathi Neotia Women and Child care Center, Kolkata
Premises no.27-0327, Street No: 327. Action Area 1D, New Town, Kolkata, West Bengal - 700156
THU
09:00 AM - 10:00 AM

Genome The Fertility Centre, Garia Main Road
Mahamayatala, Mahamayatola 228 Bus Stop, Opp Petrol Pump, 168 Garia Main Road, Kolkata, West Bengal - 700084
MON, WED, FRI
08:30 AM - 09:30 AM
Achievements & Contributions
- Dasgupta S, Chaudhury K, Mukherjee K. Usefulness of chorionic villus sampling for prenatal diagnosis of thalassaemia: a clinical study in eastern India. Int J Reprod Contracept Obstet Gynecol 2015 Jun; 4(3):790-794.
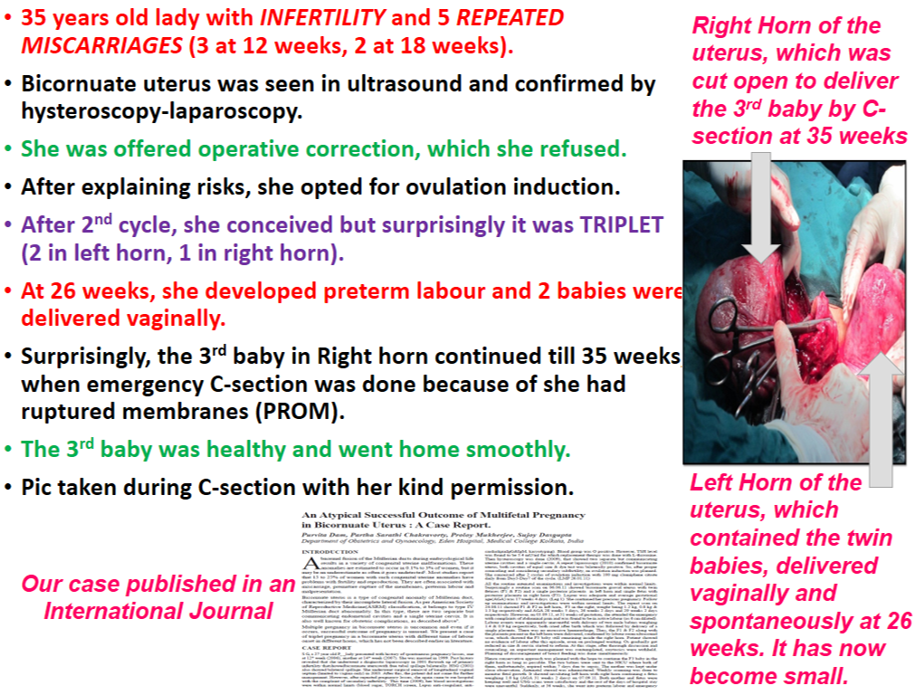
- Dam P, Chakravorty PS, Mukherjee P, Dasgupta S. An Atypical Successful Outcome of Multifetal Pregnancy in Bicornuate Uterus: A Case Report. J Int Med Sci Academ Oct-Dec 2014; 27 (4) : 211-212.
- Ghosh I, Mittal S, Banerjee D, Singh P, Dasgupta S, Chatterjee S, Biswas J, Panda C, Basu P. Study of accuracy of colposcopy in VIA and HPV detection-based cervical cancer screening program. Aus N Z J Obstet Gynaecol 2014; 54: 570–575 DOI: 10.1111/ajo.12282 PMID: 25476810.
- Dasgupta S, Mukherjee K, Chaudhury K. Risk of miscarriage following chorionic villus sampling on 315 cases for prenatal diagnosis of Thalassemia. BJOG. EP3.07. DOI: 10.1111/1471-0528.12778: 29-30.
- Dam P, Dasgupta S, Das N, Chakravorty PS. Evaluation of Role of Intrauterine Insemination in Infertility in a Tertiary Care Hospital. J of Evolution of Med and Dent Sci 2014 Apr 21; 3 (16): 4337-4348.
- Dasgupta S. Incisional Hernia in Pregnancy: A Review. Int Med J of Students' Research 2012 Jan; 2 (1): 18-23.
- Dasgupta S. An Unusual Association of Lung and Ovarian Malignancy in a Young Nonsmoker Female. Int J of User-Driven Healthcare 2012 Oct-Dec; 2(4): 20-28.
- Biswas T, Sen P, Dasgupta S, Guha Niyogi S, Ghosh GC, Bera K, Biswas R. Creating Secondary Learning Resources from BMJ Case Reports through Medical Student Conversational Learning in a Web Based Forum: A Young Man with Fever and Lymph Node Enlargement. Int J of User-Driven Healthcare 2011 Jul-Sept; 1(3): 7-19.
- Dasgupta S. Unexplained Infertility- An Enigma of reproductive Medicine. Asian Students' Med J 2011 May; 6(6).
- Basu P, Dasgupta S, Singh P. "Screening of Cervical Cancer" in Screening in Obstetrics and Gynaecology: Management of Abnormality. Pandey A, Magon N Eds. FOGSI Publication: Jaypee 2015 p135-146.
- Dasgupta S, Banerjee Ray P. Association between ophthalmoscopic changes and obstetric outcomes in preeclampsia and eclampsia. Int J Reprod Contracept Obstet Gynecol 2015 Dec; 4(6): 1944-1949.
- Dasgupta S, Sarkhel A, Jain A. Single Loading Dose of Magnesium Sulphate in Severe Preeclampsia and Eclampsia-Is it Effective? A Randomized Prospective Study. Obstet Gynecol Int J 2015 Sept, 2(6)
- Dasgupta S. Salpingectomy should be done routinely during hysterectomy. BOGS Times 2015 July: 7 (1); 6-7.
- Banerjee, D, Singh, P, Dasgupta, S, Mandal, R, Basu, P, Biswas, A phase II randomised trial evaluating concomitant immunotherapy and radiation therapy for stage-III cervical cancer. BJOG 2014 Mar; 121 (S2): 197
- Bhattacharya S, Dasgupta S, Pramanik S, Ghosh P. Primary clear cell adenocarcinoma of vagina - not associated with diethylstilbestrol exposure. Int J Reprod Contracept Obstet Gynecol 2016 Nov;5(11):4061-4063.
- Dasgupta S. Adherence to WHO 2010 Recommendations in Relation to Semen Analysis Reports in the Laboratories of West Bengal. Fertil Reprod, 2019 1(4) :187-192.
- Gold Medal in Biochemistry, 1st Professional MBBS
- Gold Medal in Pharmacology, 2nd Professional MBBS
- Gold Medal in Otorhinolaryngology (ENT), 3rd Professional MBBS Part I
- Gold Medal in Obstetrics and Gynaecology, 3rd Professional MBBS Part II
- Gold Medal in Obstetrics and Gynaecology for being selected as "Best PG Student" in MS, Obstetrics and Gynaecology
- Mcnamar Silver Medal in Biochemistry in 1st Professional MBBS
- Sutherland Silver Medal in Forensic Medicine and Toxicology in 2nd Professional MBBS
- Senior Class Assistant (The "Best Student") in Biochemistry
- Senior Class Assistant (The "Best Student") in Pharmacology
- Senior Class Assistant (The "Best Student") in ENT
- Senior Class Assistant (The "Best Student") in Paediatric Medicine
- 1st Certificate of Honours in Physiology in 1st Professional MBBS
- Honours (80.1% marks) in Biochemistry
- Honours (80% marks) in Pharmacology
- Honours (77% marks) in ENT
- Kunj-Kusum Scholarship for securing the FIRST position in 2nd Professional MBBS Examination among the students of the college
- Highest Marks in the University in Biochemistry
- Highest Marks in the College in Pharmacology
- Highest Marks in the College in ENT
- Dr Saroj Bhattacharya Memorial Award in Obstetrics and Gynaecology in 3rd Professional MBBS Part II
- 1st Prize in Case Presentation in BOGSCON - "An Atypical Outcome of Multifetal Pregnancy in Bicornuate Uterus"
- 2nd Prize in AICC-RCOG Quiz in Pune, on "Medical Disorders in pregnancy"
- Champion, Late Smt Birangana Devi Oration Competetion, Conference on Recent Trends in Cancer Research, Early Diagnosis, Prevention & Therapy "The Accuracy of Diagnostic Colposcopy using IFCPC 2011 Classification in Women Screened by VIA and HPV DNA Test"
- 1st Prize, Oral Paper Presentation, 9th Annual Conference of ISCCP "The Accuracy of IFCPC 2011 Classification to Detect Cervical Neoplasia"
- Prof Geoffrey Chamberlain Award, RCOG World Congress, London, 2019
- Honours (75% marks) in Forensic Medicine and Toxicology
- Stood third in 3rd Professional MBBS Examination Part II
- Stood first among the students of the college in MS (Obstestrics and Gynaecology) Examination
- Invited Panelist at Panel Discussion, Plexus, Annual Fest of KPC Medical College, 2011 "Occupational Hazard among Health Care Providers"
- Invited Faculty at Scientific Programme of MCESA, 2014 "Obstetric Critical Care"
- Quiz Master of Scientific Programme, MCESA, 2014
- Workshop Coordinator, ISCCP ANnual Conference, 2014
- Invited Faculty at Live Workshop on Colposcopy and Manegement of Cervical Precancers, CNCI, April 2014; August 2014; December 2014; July 2015
- Invited Faculty at Scientific Programme in BOGSCON, 2015 "Thromboprophylaxis in Obstetrics"
- Invited Faculty at Scientific Programme in MCESA, 2015 "Thromboprophylaxis in Pregnancy"
- Quiz Master in Scientific Programme of MCESA, 2015
- Examiner, Vivavoce Table, FORCE 2015
- Quiz Master, Retrocon, 2015
- CME of Medical Education and research Committee, BOGS, 2015
- Chairperson in a session, Endogyn, 2015
- Chairperson in a session, Annual Conference of South Kolkata Medical Association, IMA, 2015
- An Atypical Outcome Of Multifoetal Gestation In Bicornuate Uterus 1st prize in BOGSCON, 2012 January, 2012 ECOHUB Conclave, Kolkata
- Prevalence And Significance Of Anti-Phospholipid Antibodies In Selected At-Risk Obstetric Cases: A Comparative Prospective Study East Zone Yuva FOGSI May, 2012 Hotel Hindusthan International, Kolkata
- Management Of Overt Diabetes Before, During And After Pregnancy June, 2012 Eden Hospital Seminar Room
- Perineal Injury In Obstetrics- Prevention And Management. August, 2012 Eden Hospital Seminar Room
- Operative Vaginal Delivery- Is It A Lost Art? October, 2012 Eden Hospital Seminar Room.
- Evaluation of Role of Intrauterine Insemination (IUI) in Infertility ART-AIM Update October, 2013 Hyatt Regency, HKolkata
- The Accuracy of Diagnostic Colposcopy using IFCPC 2011 Terminology BOGSCON, 2014. January, 2014 ITC Sonar, Kolkata
- The Accuracy of Diagnostic Colposcopy using IFCPC 2011 Classification in Women Screened by VIA and HPV DNA Test Champion in Late Smt Birangana Devi Oration Competition February, 2014 CNCI., Kolkata
- The Accuracy of IFCPC 2011 Classification to Detect Cervical. Neoplasias 1st prize in 9th Annual Conference of ISCCP, 2014 February, 2014 Hotel Hindusthan International, Kolkata
- Growing Teratoma Syndrome- More Questions Than Answers BOGS Clinical Meeting June, 2014 Medical College, Kolkata
- Rate of Miscarriage Following Chorionic Villus Sampling on 315 for Prenatal Diagnosis of Thalassaemia http://epostersonline.com/rcog2014/?q=node/3040 RCOG World Congress, 2014 HICC, Hyderabad March, 2014
- Invited Panelist in a Panel Discussion on "Saving Mothers" in a CME by BOGS Committee of Safe Motherhood, at Medical College Kolkata, 2015
- Invited Faculty at East Zone Yuva FOGSI 2015 held at Puri- "Prophylactic Salpingectomy"
- Invited Speaker, "Prophylactic Salpingectomy"- East Zone Yuva FOGSI, Puri, 2015
- Invited Expert Panelist, "High Risk Pregnancy", "Why Mothers Die" International Conference, Kolkata 2015
- Invited Speaker- "Management of Sexually Transmitted Diseases", BOGSCON 2016
- Invited Quiz Master, Mediquiz, Scientific Programme of 82nd Reunion of Medical College Kolkata- 2016
- Peer Reviwer of BMJ Case Reports
- Managing Committee Member of BOGS (The Bengal Obstetric & Gynaecological Society), 2016-17, 2017-18, 2018-19, 2019-20
- Live member of FOGSI (Federation of Obstetric & Gynaecological Societies of India)
- Member of IAGE (Indian Association of Gynaecological Endoscopists)
- Live Member of IMA (Indian Medical Association)
- Active Member of MCESA (Medical College Ex-Students’ Association)
- Active Member of JVAA (Jadavpur Vidyapith Alumni Association)
- Secretary, Publication, Website and Buletin Committee, BOGS, 2015-16
- Secretary, Medical Education and Research Committee, BOGS, 2014-15
- Cultural Secretary, JVAA, 2013-2014, 2014-2015
- Executive Committee Member, Medical College Ex-Students' Association (MCESA) 2016-17, 2017-18
- Secretary, Perinatology Committee, BOGS, 2016-17
- Member of Royal College of Obstetricians and Gynaecologists (RCOG) (MRCOG), London, UK, From 2017
- Secretary, Publication, Bulltein and Website Committee BOGS 2017-18
- Secretary, Subfertility and reproductive Endocrinology Committee, BOGS, 2018-19, 2019-20
- Member, Quiz Committee, FOGSI, 2018-21
- Member, Food and Drug Committee, FOGSI, 2018-21
- Member, Endocrinology Committee, FOGSI, 2020-22
- Indian Society of Assisted Reproduction (ISAR)
- Indian fertility Society (IFS)
- Endometriosis Society of India (ESI)
- All India Coordinating Committee of Royal College of Obstetricians and Gynaecologists (AICC-RCOG)
How was your experience with Dr. Sujoy Dasgupta?
Help other patients, and let the doctor know how he's doing
Most Viewed Obstetrician and Gynecologists in Kolkata
-
DGO, DNB, MRCOG(Lon)
-
MBBS, MS(Obs & Gynae), MRCOG(London), F.I.C.R.S
26 Years Experiance
-
MBBS, DGO, MD, DNB
-
DGO, DRCOG, FPA, FRCOG
-
MBBS, DGO (Dub), DFFP (Lond), DRCOG (Lond), MRCOG (Lond), MRCP (Dub), FRCS (Edin), CSST (UK)




















































.jpg)