Heartburn
Gastroesophageal Reflux Disease (GERD)/Heartburn in ChildrenWhat is GERD?
Gastroesophageal reflux disease (GERD) is a chronic digestive disorder that is caused by the abnormal flow of gastric acid from the stomach into the esophagus.
Gastroesophageal refers to the stomach and esophagus, and reflux means to flow back or return. Gastroesophageal reflux (GER) is the return of acidic stomach juices, or food and fluids, back up into the esophagus.
GER is very common in infants, though it can occur at any age. It is the most common cause of vomiting during infancy.
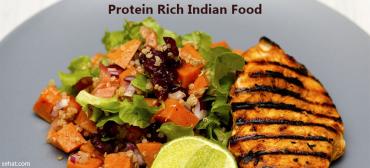
| |
| Click Image to Enlarge |
What causes GERD?
GERD is often the result of conditions that affect the lower esophageal sphincter (LES). The LES, a muscle located at the bottom of the esophagus, opens to let food into the stomach and closes to keep food in the stomach. When this muscle relaxes too often or for too long, acid refluxes back into the esophagus, causing vomiting or heartburn.
Everyone has gastroesophageal reflux from time to time. If you have ever burped and had an acid taste in your mouth, you have had reflux. The lower esophageal sphincter occasionally relaxes at inopportune times, and usually, all your child will experience is a bad taste in the mouth, or a mild, momentary feeling of heartburn.
Infants are more likely to experience weakness of the lower esophageal sphincter (LES), causing it to relax when it should remain shut. As food or milk is digesting, the LES opens and allows the stomach contents to go back up the esophagus. Sometimes, the stomach contents go all the way up the esophagus and the infant or child vomits. Other times, the stomach contents only go part of the way up the esophagus, causing heartburn, breathing problems, or, possibly, no symptoms at all.
Some foods seem to affect the muscle tone of the lower esophageal sphincter, allowing it to stay open longer than normal. These include, but are not limited to, the following:
-
Chocolate
-
Peppermint
-
High-fat foods
Other foods increase acid production in the stomach, including:
-
Citrus foods
-
Tomatoes and tomato sauces
Why is GERD a concern?
Some infants and children who have GER may not vomit, but may still have stomach contents move up the esophagus and spill over into the windpipe (the trachea). This can cause asthma, pneumonia, and possibly even SIDS (sudden infant death syndrome).
Infants and children with GERD who vomit frequently may not gain weight and grow normally. Inflammation (esophagitis) or ulcers (sores) can form in the esophagus due to contact with stomach acid. These can be painful and also may bleed, leading to anemia (too few red blood cells in the bloodstream). Esophageal narrowing (stricture) and Barrett's esophagus (abnormal cells in the esophageal lining) are long-term complications from inflammation that are seen in adults.
What are the symptoms of GERD?
Heartburn, also called acid indigestion, is the most common symptom of GERD. Heartburn is described as a burning chest pain that begins behind the breastbone and moves upward to the neck and throat. It can last as long as two hours and is often worse after eating. Lying down or bending over after a meal can also contribute to heartburn. Most children younger than 12 years of age who are diagnosed with GERD will experience a dry cough, asthma symptoms, or trouble swallowing, instead of classic heartburn.
The following are other common symptoms of GERD. However, each child may experience symptoms differently. Symptoms may include:
-
Belching
-
Refusal to eat
-
Stomachache
-
Fussiness around mealtimes
-
Frequent vomiting
-
Hiccups
-
Gagging
-
Choking
-
Frequent cough
-
Coughing fits at night
-
Wheezing
-
Frequent upper respiratory infections (colds)
-
Frequent ear infections
-
Rattling in the chest
-
Frequent sore throat in the morning
-
Sour taste in the mouth
The symptoms of GERD may resemble other conditions or medical problems. Consult your child's doctor for a diagnosis.
How is GERD diagnosed?
Your child's doctor will perform a physical examination and obtain a medical history. Diagnostic procedures that may be done to help evaluate GERD include:
-
Chest X-ray. A diagnostic test to look for evidence aspiration -- the movement of stomach contents into the lungs.
-
Upper GI (gastrointestinal) series. A diagnostic test that examines the organs of the upper part of the digestive system: the esophagus, stomach, and duodenum (the first section of the small intestine). A fluid called barium (a metallic, chemical, chalky liquid used to coat the inside of organs so that they will show up on an X-ray) is swallowed. X-rays are then taken to evaluate the digestive organs for evidence of ulceration or abnormal blockages.
-
Endoscopy. A test that uses a small, flexible tube with a light and a camera lens at the end (endoscope) to examine the inside of part of the digestive tract. Tissue samples from inside the digestive tract may also be taken for examination and testing.
-
Esophageal manometric study. A test that helps determine the strength of the muscles in the esophagus. It is useful in evaluating gastroesophageal reflux and swallowing abnormalities. A small tube is guided into the nostril, then passed into the throat, and finally into the esophagus. The pressure the esophageal muscles produce is then measured.
-
pH monitoring. To measure the acidity inside of the esophagus. It is helpful in evaluating the extent of GERD. A thin plastic tube is placed into a nostril, guided down the throat, and then into the esophagus. The tube stops just above the lower esophageal sphincter, which is at the connection between the esophagus and the stomach. The end of the tube inside the esophagus contains a sensor that measures pH, or acidity. The other end of the tube outside the body is connected to a monitor that records the pH levels for a 24- to 48-hour period. Normal activity is encouraged during the study, and a diary is kept of symptoms experienced, or activity that might be suspicious for reflux, such as gagging or coughing. It is also recommended to keep a record of the time, type, and amount of food eaten. The pH readings are evaluated and compared with the patient's activity for that time period to help determine possible GERD triggers.
-
Gastric emptying study. A test designed to determine if the stomach releases its contents into the small intestine properly. Delayed gastric emptying can contribute to reflux into the esophagus
Treatment for GERD
Specific treatment will be determined by your child's doctor based on the following:
-
Your child's age, overall health, and medical history
-
Extent of the disease
-
Your child's tolerance for specific medications, procedures, or therapies
-
The expectations for the course of the disease
-
Your opinion or preference
In many cases, GERD can be relieved through diet and lifestyle changes, under the direction of your child's physician. Some ways to better manage GERD symptoms include the following:
-
Ask your child's physician to profile any of the medications he/she is taking -- some may irritate the lining of the stomach or esophagus.
-
Watch your child's food intake -- limit fried and fatty foods, peppermint, chocolate, drinks with caffeine (such as colas, Mountain Dew, and tea), citrus fruit and juices, and tomato products.
-
Offer your child smaller portions at mealtimes, and include small snacks in-between meals if your child is hungry. Avoid letting your child overeat. Allow him or her to let you know when he or she is hungry or full.
-
If your child is overweight, consult his or her doctor to set weight loss goals.
-
Do not allow your child to lie down or go to bed right after a meal. Serve the evening meal early -- at least two hours before bedtime. Always remember to check with your infant's doctor before elevating the head of the crib if he or she has been diagnosed with gastroesophageal reflux. This is for safety reasons and to reduce the risk for SIDS and other sleep-related infant deaths.
-
After feedings, hold your infant in an upright position for 30 minutes.
-
If bottle-feeding, keep the nipple filled with milk so your infant does not swallow too much air while eating. Try different nipples to find one that allows your baby's mouth to make a good seal with the nipple during feeding.
-
Adding rice cereal to feeding may be beneficial for some infants.
-
Burp your baby several times during bottle- or breast-feeding. Your child may reflux more often when burping with a full stomach.
Treatment may include:
-
Medications. If needed, your child's doctor may prescribe medications to help with reflux. There are medications which help decrease the amount of acid the stomach makes, which, in turn, will cut down on the heartburn associated with reflux. One group of this type of medication is called "H2-blockers." Medications in this category include cimetidine (Tagamet) and ranitidine (Zantac). Another group of medications is called "proton-pump inhibitors." Medications in this category include omeprazole (Prilosec) and lansoprazole (Prevacid). These medications are taken daily to prevent excess acid secretion in the stomach.
Another type of medicine your child's doctor may prescribe helps the stomach empty faster. If food does not remain in the stomach as long as usual, there may be less chance of reflux occurring. A medicine in this category that can be prescribed is metoclopramide (Reglan). This medicine is usually taken three to four times a day, before meals or feedings, and at bedtime.
-
Calorie supplements. Some infants with reflux will not be able to gain weight due to frequent vomiting. Your child's doctor may recommend the following:
-
Adding rice cereal to baby formula
-
Providing your infant with more calories by adding a prescribed supplement (such as Polycose or Moducal) to formula or breast milk to make the milk higher in calories than normal
-
Change formula to milk- or soy-free formula if allergy is suspected
-
-
Tube feedings. Some babies with reflux have other conditions that make them tired, such as congenital heart disease or prematurity. In addition to having reflux, these babies may not be able to eat or drink very much without becoming sleepy. Other babies are not able to tolerate a normal amount of formula in the stomach without vomiting, and would do better if a small amount of milk was given continuously. In both of these cases, tube feedings may be recommended. Formula or breast milk is given through a tube that is placed in the nose, guided through the esophagus, and into the stomach (nasogastric tube). Nasogastric tube feedings can be given in addition to or instead of what a baby takes from a bottle. Nasoduodenal tubes can also be used to bypass the stomach.
-
Surgery. In severe cases of reflux, a surgical procedure called fundoplication may be performed. Your doctor may recommend this operation if your child is not gaining weight due to vomiting, has frequent respiratory problems, or has severe irritation in the esophagus. This procedure is usually done laparoscopically, which means that pain in minimized and the recovery time is faster after surgery. Small incisions are made in the abdomen, and a small tube with a camera on the end is placed into one of the incisions to look inside. The surgical instruments are placed through the other incisions while the surgeon looks at a video monitor to see the stomach and other organs. The top portion of the stomach is wrapped around the esophagus, creating a tight band that reinforces the lower esophageal sphincter and greatly decreases reflux.
What is the long-term outlook for a child with GERD?
Many infants who vomit will "outgrow it" by the time they are about a year old, as the lower esophageal sphincter becomes stronger. For others, medications, lifestyle, and diet changes can minimize reflux, vomiting, and heartburn.