How Communities Are Changing the Way We Think About Aging in..
8 Min Read
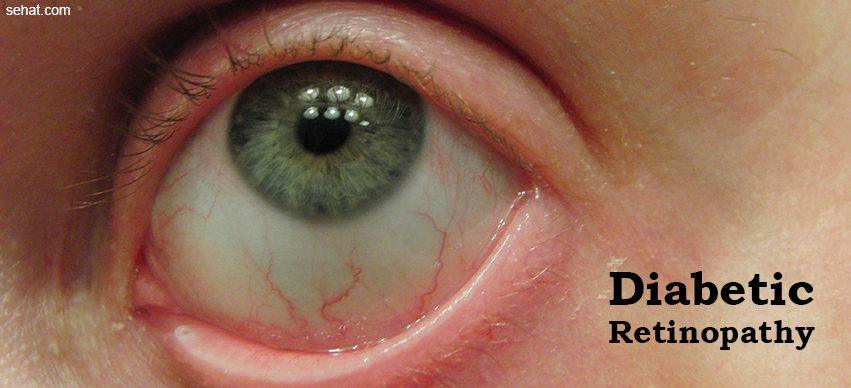

Diabetic retinopathy is a diabetes complication that results due the changes in blood vessels of the retina caused by high blood sugar levels. This complication can lead to blurring of vision, subconjunctival hemorrhage, and if left untreated, even blindness.
Though these symptoms are not always indicators of diabetic retinopathy, if you are diabetic, ensure you consult your eye doctor for an examination every year, even if you don’t experience these symptoms. If you are pregnant, especially, high blood pressure can trigger diabetic retinopathy, so exercise caution.
The longer you have been suffering from diabetes, the more susceptible you are to diabetic retinopathy. Diabetic patients are 25 times more prone to blindness as compared to the general population. Therefore, it is important for diabetics to keep their blood sugar in check and visit the eye doctor regularly for a diabetic eye exam. Following are the most common risk factors of diabetic retinopathy:
NPDR is the early onset of diabetic retinopathy, which is characterised by mild or no symptoms. Here, the retinal blood vessels get weak and the tiny bulges in the blood vessels, known as micro aneurysms may leak fluid into the retina. As a result, the macula may get swollen up.
PDR is the advanced stage of diabetic retinopathy that is characterised by the deprivation of oxygen in the retina caused due to poor circulation. New and weak blood vessels start to grow in the retina and the vitreous. The new blood vessels may cause leakage of blood into the vitreous, thereby hindering clear vision.
Vitreous haemorrhage is caused when blood seeps into the eye’s clear vitreous gel due to damage to the blood vessels of the retina. This can lead to blurred vision, appearance of a few dark spots and in extreme cases, even vision loss.
In diabetic macular edema, the retinal blood vessels develop small leaks which cause the blood, fluid and fatty material to get deposited in the retina. This results in the swelling of retina, which subsequently impairs vision.
Diabetic retinopathy can cause abnormal changes in blood vessels that can trigger the growth of scar tissue. The scar tissue can detach the retina form its position, causing floating in the vision or vision loss.
Diabetic retinopathy may also lead to the growth of new blood vessels in the front part of the eye, thereby obstructing the normal flow of fluid out of the eye and putting pressure in the eye to build up. The optic nerve that transmits images from the eye to the brain can get damaged due to this pressure.
Diabetic retinopathy, if left uncontrolled, can lead to partial or complete vision loss.
Going for regular diabetes eye tests and strictly maintaining blood sugar and blood pressure levels can help a great deal in the prevention of diabetic retinopathy. Though in mild cases of the disease, treatment is not required, in severe cases, doctors recommend the following treatments to prevent vision loss and correct existing vision impairment:
Focal laser surgery halts the leakage of blood and fluid in the eye. While this surgery might not help correct blurred vision caused by macular edema before surgery, it can prevent the further progression of macular edema.
Scatter laser surgery helps shrink the abnormal blood vessels that develop as a result of diabetic retinopathy. You may experience a slight loss of peripheral vision or night vision after the surgery.
Intraocular steroid injection helps treat diabetic macular edema by reducing the leakage of fluid into the retina and, therefore, improving vision. Since diabetes eye disease is a chronic condition, you may require to repeat this treatment or combine it along with laser surgery for better results.
Vitrectomy is recommended by doctors for advanced cases of diabetic retinopathy. In this procedure, a small incision in the eye is used to remove blood from the middle of the eye as well as the scar tissue pulling the retina.